Continuous Fenestrated and Sinusoidal Describe a Type of Capillary
General Characteristics
Definition
Capillaries are the smallest of the blood vessels. Capillaries are the primary structures in the circulatory system that allow the exchange of gas, nutrients, and other materials between the blood and the extracellular fluid Extracellular fluid The fluid of the body that is outside of cells. It is the external environment for the cells. Body Fluid Compartments (ECF).
Structure
- Simple tubes made up of a single layer of endothelial cells
- Diameter:
- Approximately 5 µm in diameter at the arterial end
- Approximately 9 µm in diameter at the venous end
- RBCs RBCs Erythrocytes, or red blood cells (RBCs), are the most abundant cells in the blood. While erythrocytes in the fetus are initially produced in the yolk sac then the liver, the bone marrow eventually becomes the main site of production. Erythrocytes: Histology are approximately 7 µm in diameter → RBCs RBCs Erythrocytes, or red blood cells (RBCs), are the most abundant cells in the blood. While erythrocytes in the fetus are initially produced in the yolk sac then the liver, the bone marrow eventually becomes the main site of production. Erythrocytes: Histology are forced through capillaries 1 at a time
- Endothelial cells are separated from surrounding tissue by basal lamina.
- Capillaries are surrounded by pericytes (epithelial cells within the endothelial basal lamina, which play a role in neurovascular signaling).
- Arranged in vast networks known as capillary beds (groups of 10–100 individual capillary vessels supplied by a single metarteriole)
- Massive total surface area: estimated at > 6,300 m2
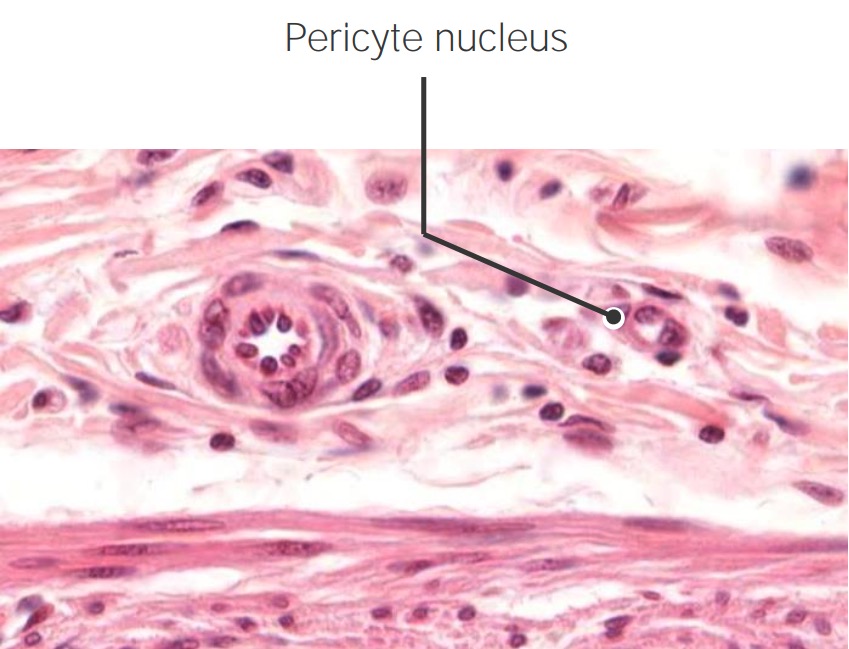
Cross-section of an arteriole (left) and a capillary (right) with a surrounding pericyte (labeled pericyte nucleus Nucleus Within a eukaryotic cell, a membrane-limited body which contains chromosomes and one or more nucleoli (cell nucleolus). The nuclear membrane consists of a double unit-type membrane which is perforated by a number of pores; the outermost membrane is continuous with the endoplasmic reticulum. A cell may contain more than one nucleus. The Cell: Organelles )
Image by Geoffrey Meyer, PhD.Blood flow Blood flow Blood flow refers to the movement of a certain volume of blood through the vasculature over a given unit of time (e.g., mL per minute). Vascular Resistance, Flow, and Mean Arterial Pressure through and around capillaries
- Blood enters the capillary beds through the arterioles Arterioles The smallest divisions of the arteries located between the muscular arteries and the capillaries. Arteries: Histology → metarterioles Metarterioles Short vessels linking arterioles and capillaries. Arteries: Histology → capillaries
- Blood drains into the thoroughfare channel → venules Venules The minute vessels that collect blood from the capillary plexuses and join together to form veins. Veins: Histology
- Metarterioles Metarterioles Short vessels linking arterioles and capillaries. Arteries: Histology contain precapillary sphincters of smooth muscle at the entrance to each individual capillary:
- Regulate the amount of blood flow Blood flow Blood flow refers to the movement of a certain volume of blood through the vasculature over a given unit of time (e.g., mL per minute). Vascular Resistance, Flow, and Mean Arterial Pressure into the capillary bed
- When sphincters are closed, blood bypasses the capillaries and flows straight into the thoroughfare channel.
- Arteriovenous (AV) anastomoses/shunts: Vessels bypass the capillary beds and directly connect arteries Arteries Arteries are tubular collections of cells that transport oxygenated blood and nutrients from the heart to the tissues of the body. The blood passes through the arteries in order of decreasing luminal diameter, starting in the largest artery (the aorta) and ending in the small arterioles. Arteries are classified into 3 types: large elastic arteries, medium muscular arteries, and small arteries and arterioles. Arteries: Histology and veins Veins Veins are tubular collections of cells, which transport deoxygenated blood and waste from the capillary beds back to the heart. Veins are classified into 3 types: small veins/venules, medium veins, and large veins. Each type contains 3 primary layers: tunica intima, tunica media, and tunica adventitia. Veins: Histology .
- AV shunts are present when precapillary sphincters are closed.
- Numerous in the dermis Dermis A layer of vascularized connective tissue underneath the epidermis. The surface of the dermis contains innervated papillae. Embedded in or beneath the dermis are sweat glands; hair follicles; and sebaceous glands. Skin: Structure and Functions (help regulate body heat Heat Inflammation )
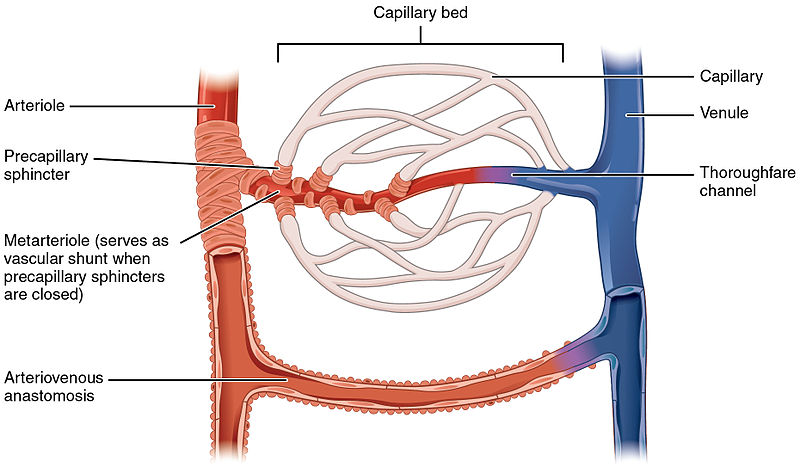
Capillary bed demonstrating arteriole, metarteriole, and precapillary sphincters
Image: "Capillary bed" by OpenStax College. License: CC BY 3.0Location
- Capillaries are the connection between the smallest arteries Arteries Arteries are tubular collections of cells that transport oxygenated blood and nutrients from the heart to the tissues of the body. The blood passes through the arteries in order of decreasing luminal diameter, starting in the largest artery (the aorta) and ending in the small arterioles. Arteries are classified into 3 types: large elastic arteries, medium muscular arteries, and small arteries and arterioles. Arteries: Histology ( arterioles Arterioles The smallest divisions of the arteries located between the muscular arteries and the capillaries. Arteries: Histology ) and the smallest veins Veins Veins are tubular collections of cells, which transport deoxygenated blood and waste from the capillary beds back to the heart. Veins are classified into 3 types: small veins/venules, medium veins, and large veins. Each type contains 3 primary layers: tunica intima, tunica media, and tunica adventitia. Veins: Histology ( venules Venules The minute vessels that collect blood from the capillary plexuses and join together to form veins. Veins: Histology ).
- Found within 60–80 µm of essentially every cell in the body
- Capillary beds are located in all tissues except:
- Cartilage Cartilage Cartilage is a type of connective tissue derived from embryonic mesenchyme that is responsible for structural support, resilience, and the smoothness of physical actions. Perichondrium (connective tissue membrane surrounding cartilage) compensates for the absence of vasculature in cartilage by providing nutrition and support. Cartilage: Histology
- Epithelia
- Eye cornea Cornea The transparent anterior portion of the fibrous coat of the eye consisting of five layers: stratified squamous corneal epithelium; bowman membrane; corneal stroma; descemet membrane; and mesenchymal corneal endothelium. It serves as the first refracting medium of the eye. Eye: Anatomy and lens Lens A transparent, biconvex structure of the eye, enclosed in a capsule and situated behind the iris and in front of the vitreous humor (vitreous body). It is slightly overlapped at its margin by the ciliary processes. Adaptation by the ciliary body is crucial for ocular accommodation. Eye: Anatomy
- Tendons and ligaments have some capillaries, but much less than most other tissue.
Physiology
- Functions:
- Gas exchange Gas exchange Human cells are primarily reliant on aerobic metabolism. The respiratory system is involved in pulmonary ventilation and external respiration, while the circulatory system is responsible for transport and internal respiration. Pulmonary ventilation (breathing) represents movement of air into and out of the lungs. External respiration, or gas exchange, is represented by the O2 and CO2 exchange between the lungs and the blood. Gas Exchange : Oxygen exits RBCs RBCs Erythrocytes, or red blood cells (RBCs), are the most abundant cells in the blood. While erythrocytes in the fetus are initially produced in the yolk sac then the liver, the bone marrow eventually becomes the main site of production. Erythrocytes: Histology , carbon dioxide enters RBCs RBCs Erythrocytes, or red blood cells (RBCs), are the most abundant cells in the blood. While erythrocytes in the fetus are initially produced in the yolk sac then the liver, the bone marrow eventually becomes the main site of production. Erythrocytes: Histology .
- Nutrient delivery
- Blood picks up cellular and interstitial waste.
- Mechanisms of exchange:
- Transcytosis/ pinocytosis Pinocytosis The engulfing of liquids by cells by a process of invagination and closure of the cell membrane to form fluid-filled vacuoles. Pharmacokinetics and Pharmacodynamics : Substances are taken into the endothelial cells in vesicles Vesicles Female Genitourinary Examination via endocytosis Endocytosis Cellular uptake of extracellular materials within membrane-limited vacuoles or microvesicles. Endosomes play a central role in endocytosis. The Cell: Cell Membrane , transported across the cell, and released on the other side.
- Direct filtration: relies on Starling forces
- Starling forces applied to capillaries:
- Relatively higher hydrostatic pressure Hydrostatic pressure The pressure due to the weight of fluid. Edema in the arterioles Arterioles The smallest divisions of the arteries located between the muscular arteries and the capillaries. Arteries: Histology pushes fluid, nutrients, and other cellular material into the surrounding ECF.
- Plasma Plasma The residual portion of blood that is left after removal of blood cells by centrifugation without prior blood coagulation. Transfusion Products proteins Proteins Linear polypeptides that are synthesized on ribosomes and may be further modified, crosslinked, cleaved, or assembled into complex proteins with several subunits. The specific sequence of amino acids determines the shape the polypeptide will take, during protein folding, and the function of the protein. Energy Homeostasis generally cannot pass through the capillary walls → plasma Plasma The residual portion of blood that is left after removal of blood cells by centrifugation without prior blood coagulation. Transfusion Products oncotic pressure Oncotic Pressure Edema ↑ towards the venous end of the capillary
- Relatively higher oncotic pressure Oncotic Pressure Edema in the venules Venules The minute vessels that collect blood from the capillary plexuses and join together to form veins. Veins: Histology allows waste to be absorbed into the vessels
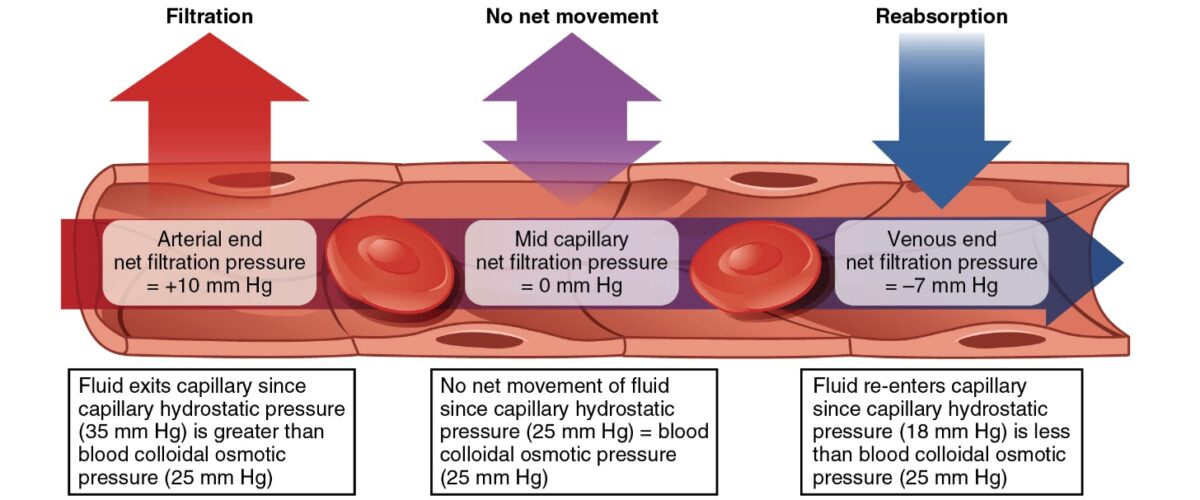
Starling forces:
Starling forces within a capillary determine the flow Flow Blood flows through the heart, arteries, capillaries, and veins in a closed, continuous circuit. Flow is the movement of volume per unit of time. Flow is affected by the pressure gradient and the resistance fluid encounters between 2 points. Vascular resistance is the opposition to flow, which is caused primarily by blood friction against vessel walls. Vascular Resistance, Flow, and Mean Arterial Pressure of molecules into and out of the vessel.
Types of Capillaries
3 primary types of capillaries:
- Continuous capillaries
- Fenestrated capillaries
- Sinusoid, or discontinuous, capillaries
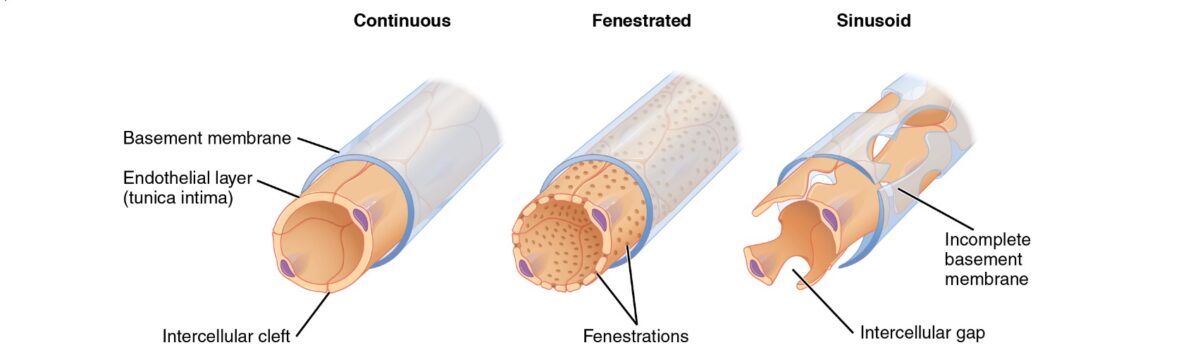
Types of capillaries
Image: "Types of capillaries" by Phil Schatz. License: CC BY 4.0Continuous capillaries
Continuous capillaries are the most common type of capillary.
- Structure:
- Endothelial cells are connected via occluding tight junctions Tight junctions Cell-cell junctions that seal adjacent epithelial cells together, preventing the passage of most dissolved molecules from one side of the epithelial sheet to the other. The Cell: Cell Junctions .
- Continuous basal lamina
- Prevents diffusion Diffusion The tendency of a gas or solute to pass from a point of higher pressure or concentration to a point of lower pressure or concentration and to distribute itself throughout the available space. Diffusion, especially facilitated diffusion, is a major mechanism of biological transport. Peritoneal Dialysis and Hemodialysis of fluid, protein, and other molecules
- Some tissues contain small clefts (approximately 4 nm wide) → allow the passage of very small molecules (e.g., glucose Glucose A primary source of energy for living organisms. It is naturally occurring and is found in fruits and other parts of plants in its free state. It is used therapeutically in fluid and nutrient replacement. Lactose Intolerance )
- Primary mechanism of exchange: transcytosis/ pinocytosis Pinocytosis The engulfing of liquids by cells by a process of invagination and closure of the cell membrane to form fluid-filled vacuoles. Pharmacokinetics and Pharmacodynamics
- Location (found in organs requiring passage of only select molecules):
- Central nervous system Central nervous system The main information-processing organs of the nervous system, consisting of the brain, spinal cord, and meninges. Nervous System: Anatomy, Structure, and Classification
- Lungs Lungs Lungs are the main organs of the respiratory system. Lungs are paired viscera located in the thoracic cavity and are composed of spongy tissue. The primary function of the lungs is to oxygenate blood and eliminate CO2. Lungs: Anatomy
- All muscle: cardiac Cardiac Total Anomalous Pulmonary Venous Return (TAPVR) , skeletal, and smooth
- Connective tissue Connective tissue Connective tissues originate from embryonic mesenchyme and are present throughout the body except inside the brain and spinal cord. The main function of connective tissues is to provide structural support to organs. Connective tissues consist of cells and an extracellular matrix. Connective Tissue: Histology
- Skin Skin The skin, also referred to as the integumentary system, is the largest organ of the body. The skin is primarily composed of the epidermis (outer layer) and dermis (deep layer). The epidermis is primarily composed of keratinocytes that undergo rapid turnover, while the dermis contains dense layers of connective tissue. Skin: Structure and Functions
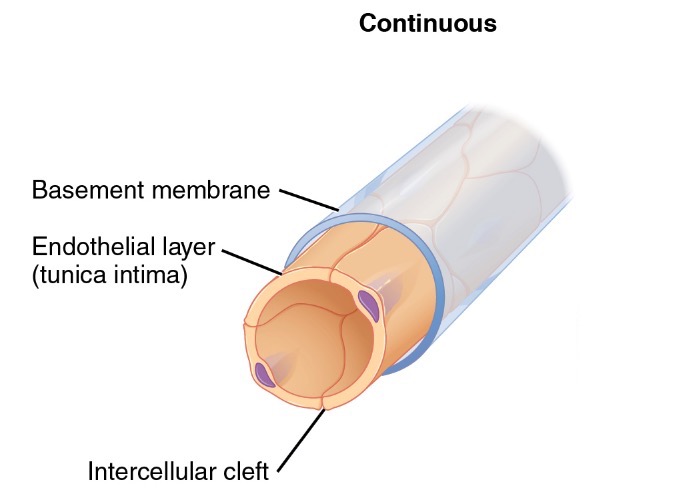
Diagram of a continuous capillary
Image: "Continuous capillaries" by Phil Schatz. License: CC BY 4.0Fenestrated capillaries
Fenestrated capillaries are important in organs requiring rapid absorption Absorption Absorption involves the uptake of nutrient molecules and their transfer from the lumen of the GI tract across the enterocytes and into the interstitial space, where they can be taken up in the venous or lymphatic circulation. Digestion and Absorption and filtration, or with high metabolic activity.
- Structure:
- Wall contains multiple fenestrations, or "pores", with continuous basal lamina.
- Fenestrations are approximately 20–100 nm in diameter.
- Allows for the rapid passage of small molecules, but keeps proteins Proteins Linear polypeptides that are synthesized on ribosomes and may be further modified, crosslinked, cleaved, or assembled into complex proteins with several subunits. The specific sequence of amino acids determines the shape the polypeptide will take, during protein folding, and the function of the protein. Energy Homeostasis and larger particles within the blood vessel
- Primary mechanism of exchange: filtration
- Location:
- Kidneys Kidneys The kidneys are a pair of bean-shaped organs located retroperitoneally against the posterior wall of the abdomen on either side of the spine. As part of the urinary tract, the kidneys are responsible for blood filtration and excretion of water-soluble waste in the urine. Kidneys: Anatomy
- Endocrine organs (e.g., pancreas Pancreas The pancreas lies mostly posterior to the stomach and extends across the posterior abdominal wall from the duodenum on the right to the spleen on the left. This organ has both exocrine and endocrine tissue. Pancreas: Anatomy )
- Intestinal tract
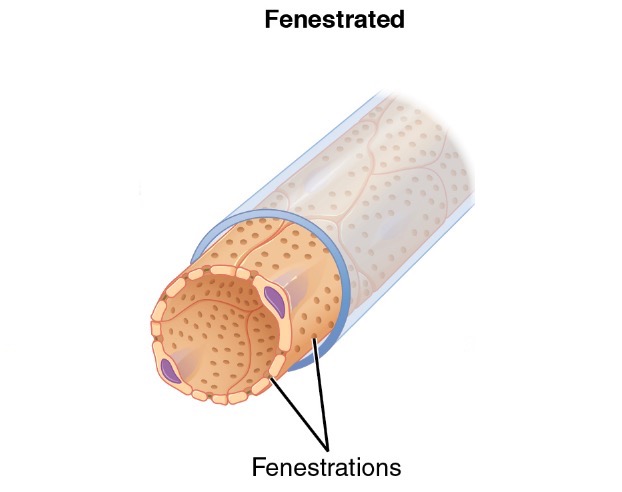
Diagram of a fenestrated capillary
Image: "Fenestrated capillaries" by Phil Schatz. License: CC BY 4.0Sinusoid (discontinuous) capillaries
Sinusoid, or discontinuous, capillaries allow larger proteins Proteins Linear polypeptides that are synthesized on ribosomes and may be further modified, crosslinked, cleaved, or assembled into complex proteins with several subunits. The specific sequence of amino acids determines the shape the polypeptide will take, during protein folding, and the function of the protein. Energy Homeostasis and full cells to pass through larger gaps.
- Structure:
- Large gaps (up to 0.5 µm) in the cytoplasm of the endothelium Endothelium A layer of epithelium that lines the heart, blood vessels (vascular endothelium), lymph vessels (lymphatic endothelium), and the serous cavities of the body. Arteries: Histology
- Basal lamina has large gaps or may be completely absent.
- May appear as larger, blood-filled spaces between other tissues
- Mechanism of exchange: direct filtration/ diffusion Diffusion The tendency of a gas or solute to pass from a point of higher pressure or concentration to a point of lower pressure or concentration and to distribute itself throughout the available space. Diffusion, especially facilitated diffusion, is a major mechanism of biological transport. Peritoneal Dialysis and Hemodialysis
- Locations:
- Liver Liver The liver is the largest gland in the human body. The liver is found in the superior right quadrant of the abdomen and weighs approximately 1.5 kilograms. Its main functions are detoxification, metabolism, nutrient storage (e.g., iron and vitamins), synthesis of coagulation factors, formation of bile, filtration, and storage of blood. Liver: Anatomy
- Spleen Spleen The spleen is the largest lymphoid organ in the body, located in the LUQ of the abdomen, superior to the left kidney and posterior to the stomach at the level of the 9th-11th ribs just below the diaphragm. The spleen is highly vascular and acts as an important blood filter, cleansing the blood of pathogens and damaged erythrocytes. Spleen: Anatomy
- Bone Bone Bone is a compact type of hardened connective tissue composed of bone cells, membranes, an extracellular mineralized matrix, and central bone marrow. The 2 primary types of bone are compact and spongy. Bones: Structure and Types marrow
- Specialized functions:
- Allows larger structures to enter circulation Circulation The movement of the blood as it is pumped through the cardiovascular system. ABCDE Assessment , for example:
- Proteins Proteins Linear polypeptides that are synthesized on ribosomes and may be further modified, crosslinked, cleaved, or assembled into complex proteins with several subunits. The specific sequence of amino acids determines the shape the polypeptide will take, during protein folding, and the function of the protein. Energy Homeostasis synthesized in the liver Liver The liver is the largest gland in the human body. The liver is found in the superior right quadrant of the abdomen and weighs approximately 1.5 kilograms. Its main functions are detoxification, metabolism, nutrient storage (e.g., iron and vitamins), synthesis of coagulation factors, formation of bile, filtration, and storage of blood. Liver: Anatomy (e.g., albumin Albumin Serum albumin from humans. It is an essential carrier of both endogenous substances, such as fatty acids and bilirubin, and of xenobiotics in the blood. Liver Function Tests and clotting factors)
- Blood synthesized in the bone Bone Bone is a compact type of hardened connective tissue composed of bone cells, membranes, an extracellular mineralized matrix, and central bone marrow. The 2 primary types of bone are compact and spongy. Bones: Structure and Types marrow
- Allows for "aggressive" communication Communication The exchange or transmission of ideas, attitudes, or beliefs between individuals or groups. Decision-making Capacity and Legal Competence between the perivascular cells and the blood itself
- Allows larger structures to enter circulation Circulation The movement of the blood as it is pumped through the cardiovascular system. ABCDE Assessment , for example:
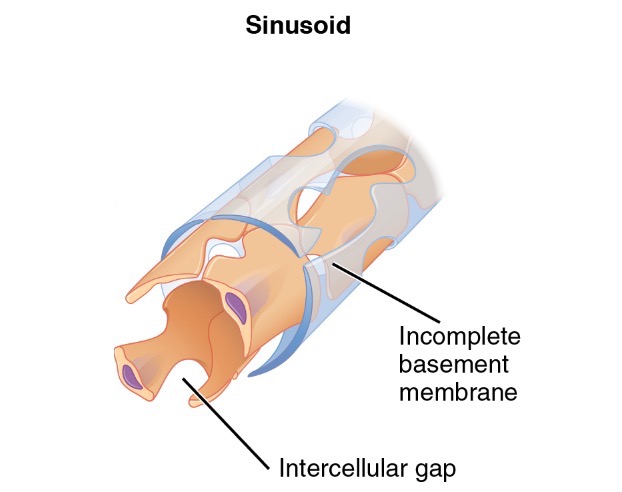
Diagram of a sinusoid capillary
Image: "Sinusoid capillaries" by Phil Schatz. License: CC BY 4.0Clinical Relevance
Thrombotic microangiopathies
Thrombotic microangiopathies (TMAs) are a group of conditions characterized by abnormalities in the walls of arterioles Arterioles The smallest divisions of the arteries located between the muscular arteries and the capillaries. Arteries: Histology and capillaries, which lead to microvascular thrombosis Thrombosis Formation and development of a thrombus or blood clot in the blood vessel. Epidemic Typhus . The most common primary TMAs are thrombotic thrombocytopenic purpura Thrombotic thrombocytopenic purpura Thrombotic thrombocytopenic purpura (TTP) is a life-threatening condition due to either a congenital or an acquired deficiency of ADAMTS-13, a metalloproteinase that cleaves multimers of von Willebrand factor (VWF). The large multimers then aggregate excessive platelets resulting in microvascular thrombosis and an increase in consumption of platelets. Thrombotic Thrombocytopenic Purpura ( TTP TTP Thrombotic thrombocytopenic purpura (TTP) is a life-threatening condition due to either a congenital or an acquired deficiency of adamts-13, a metalloproteinase that cleaves multimers of von Willebrand factor (vWF). The large multimers then aggregate excessive platelets resulting in microvascular thrombosis and an increase in consumption of platelets. Thrombotic Thrombocytopenic Purpura ) and hemolytic uremic syndrome Hemolytic uremic syndrome A syndrome that is associated with microvascular diseases of the kidney, such as renal cortical necrosis. It is characterized by hemolytic anemia; thrombocytopenia; and acute renal failure. Hypocoagulable Conditions ( HUS HUS Hemolytic uremic syndrome (HUS) is a clinical phenomenon most commonly seen in children that consists of a classic triad of microangiopathic hemolytic anemia, thrombocytopenia, and acute kidney injury. Hemolytic uremic syndrome is a major cause of acute kidney injury in children and is most commonly associated with a prodrome of diarrheal illness caused by shiga-like toxin-producing bacteria. Hemolytic Uremic Syndrome ). Drugs can also induce a TMA.
- Thrombotic thrombocytopenic purpura Thrombotic thrombocytopenic purpura Thrombotic thrombocytopenic purpura (TTP) is a life-threatening condition due to either a congenital or an acquired deficiency of ADAMTS-13, a metalloproteinase that cleaves multimers of von Willebrand factor (VWF). The large multimers then aggregate excessive platelets resulting in microvascular thrombosis and an increase in consumption of platelets. Thrombotic Thrombocytopenic Purpura : a life-threatening condition due to either a congenital Congenital Chorioretinitis or an acquired deficiency of ADAMTS-13, a metalloproteinase cleaving multimer of von Willebrand's Factor (vWF). Without metalloproteinase, the large multimers aggregate excessive platelets Platelets Platelets are small cell fragments involved in hemostasis. Thrombopoiesis takes place primarily in the bone marrow through a series of cell differentiation and is influenced by several cytokines. Platelets are formed after fragmentation of the megakaryocyte cytoplasm. Platelets: Histology , resulting in microvascular thrombosis Thrombosis Formation and development of a thrombus or blood clot in the blood vessel. Epidemic Typhus and an increase in consumption of platelets Platelets Platelets are small cell fragments involved in hemostasis. Thrombopoiesis takes place primarily in the bone marrow through a series of cell differentiation and is influenced by several cytokines. Platelets are formed after fragmentation of the megakaryocyte cytoplasm. Platelets: Histology . The classic clinical presentation Presentation The position or orientation of the fetus at near term or during obstetric labor, determined by its relation to the spine of the mother and the birth canal. The normal position is a vertical, cephalic presentation with the fetal vertex flexed on the neck. Normal and Abnormal Labor includes thrombocytopenia Thrombocytopenia Thrombocytopenia occurs when the platelet count is < 150,000 per microliter. The normal range for platelets is usually 150,000-450,000/µL of whole blood. Thrombocytopenia can be a result of decreased production, increased destruction, or splenic sequestration of platelets. Patients are often asymptomatic until platelet counts are < 50,000/µL. Thrombocytopenia , hemolytic anemia Anemia Anemia is a condition in which individuals have low Hb levels, which can arise from various causes. Anemia is accompanied by a reduced number of RBCs and may manifest with fatigue, shortness of breath, pallor, and weakness. Subtypes are classified by the size of RBCs, chronicity, and etiology. Anemia: Overview and Types , kidney disease, neurological symptoms, and fever Fever Fever is defined as a measured body temperature of at least 38°C (100.4°F). Fever is caused by circulating endogenous and/or exogenous pyrogens that increase levels of prostaglandin E2 in the hypothalamus. Fever is commonly associated with chills, rigors, sweating, and flushing of the skin. Fever .
- Hemolytic uremic syndrome Hemolytic uremic syndrome A syndrome that is associated with microvascular diseases of the kidney, such as renal cortical necrosis. It is characterized by hemolytic anemia; thrombocytopenia; and acute renal failure. Hypocoagulable Conditions : a clinical phenomenon most commonly seen in children consisting of the classic triad of microangiopathic hemolytic anemia Anemia Anemia is a condition in which individuals have low Hb levels, which can arise from various causes. Anemia is accompanied by a reduced number of RBCs and may manifest with fatigue, shortness of breath, pallor, and weakness. Subtypes are classified by the size of RBCs, chronicity, and etiology. Anemia: Overview and Types , thrombocytopenia Thrombocytopenia Thrombocytopenia occurs when the platelet count is < 150,000 per microliter. The normal range for platelets is usually 150,000-450,000/µL of whole blood. Thrombocytopenia can be a result of decreased production, increased destruction, or splenic sequestration of platelets. Patients are often asymptomatic until platelet counts are < 50,000/µL. Thrombocytopenia , and acute kidney injury Acute Kidney Injury Acute kidney injury refers to sudden and often reversible loss of renal function, which develops over days or weeks. Azotemia refers to elevated levels of nitrogen-containing substances in the blood that accompany AKI, which include BUN and creatinine. Acute Kidney Injury . Hemolytic uremic syndrome Hemolytic uremic syndrome A syndrome that is associated with microvascular diseases of the kidney, such as renal cortical necrosis. It is characterized by hemolytic anemia; thrombocytopenia; and acute renal failure. Hypocoagulable Conditions is most commonly associated with a prodrome Prodrome Symptoms that appear 24–48 hours prior to migraine onset. Migraine Headache of diarrheal illness caused by Shiga-like, toxin-producing bacteria Bacteria Bacteria are prokaryotic single-celled microorganisms that are metabolically active and divide by binary fission. Some of these organisms play a significant role in the pathogenesis of diseases. Bacteriology .
Increased hydrostatic pressure Hydrostatic pressure The pressure due to the weight of fluid. Edema within the capillaries
Any condition preventing blood flow Blood flow Blood flow refers to the movement of a certain volume of blood through the vasculature over a given unit of time (e.g., mL per minute). Vascular Resistance, Flow, and Mean Arterial Pressure from moving forward can lead to an increase in hydrostatic pressure Hydrostatic pressure The pressure due to the weight of fluid. Edema within the vessels, which ultimately may get transmitted to the capillaries. Increasing the hydrostatic pressure Hydrostatic pressure The pressure due to the weight of fluid. Edema within the capillaries affects the exchange of substances through the capillaries, pushing more fluid and substrates into the ECF. The types of conditions may include:
- Congestive heart failure Congestive heart failure Congestive heart failure refers to the inability of the heart to supply the body with normal cardiac output to meet metabolic needs. Echocardiography can confirm the diagnosis and give information about the ejection fraction. Congestive Heart Failure : the inability of the heart to supply the body with the cardiac Cardiac Total Anomalous Pulmonary Venous Return (TAPVR) output required to meet the body's metabolic needs. Patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship typically present with dyspnea Dyspnea Dyspnea is the subjective sensation of breathing discomfort. Dyspnea is a normal manifestation of heavy physical or psychological exertion, but also may be caused by underlying conditions (both pulmonary and extrapulmonary). Dyspnea on exertion and/or at rest, orthopnea Orthopnea Pulmonary Edema , and peripheral edema Edema Edema is a condition in which excess serous fluid accumulates in the body cavity or interstitial space of connective tissues. Edema is a symptom observed in several medical conditions. It can be categorized into 2 types, namely, peripheral (in the extremities) and internal (in an organ or body cavity). Edema . Because blood is not effectively pumped out of the heart, pressure builds up in venous circulation Circulation The movement of the blood as it is pumped through the cardiovascular system. ABCDE Assessment and ultimately backs up into the capillaries. Diagnosis can be made with an echocardiogram Echocardiogram Transposition of the Great Vessels .
- Cirrhosis Cirrhosis Cirrhosis is a late stage of hepatic parenchymal necrosis and scarring (fibrosis) most commonly due to hepatitis C infection and alcoholic liver disease. Patients may present with jaundice, ascites, and hepatosplenomegaly. Cirrhosis can also cause complications such as hepatic encephalopathy, portal hypertension, portal vein thrombosis, and hepatorenal syndrome. Cirrhosis : late stage of hepatic necrosis Necrosis The death of cells in an organ or tissue due to disease, injury or failure of the blood supply. Ischemic Cell Damage and scarring Scarring Inflammation . Chronic cellular damage causes extensive distortion Distortion Defense Mechanisms of the normal hepatic architecture, which can lead to impairment of normal blood flow Blood flow Blood flow refers to the movement of a certain volume of blood through the vasculature over a given unit of time (e.g., mL per minute). Vascular Resistance, Flow, and Mean Arterial Pressure through the liver Liver The liver is the largest gland in the human body. The liver is found in the superior right quadrant of the abdomen and weighs approximately 1.5 kilograms. Its main functions are detoxification, metabolism, nutrient storage (e.g., iron and vitamins), synthesis of coagulation factors, formation of bile, filtration, and storage of blood. Liver: Anatomy . The most common causes of cirrhosis Cirrhosis Cirrhosis is a late stage of hepatic parenchymal necrosis and scarring (fibrosis) most commonly due to hepatitis C infection and alcoholic liver disease. Patients may present with jaundice, ascites, and hepatosplenomegaly. Cirrhosis can also cause complications such as hepatic encephalopathy, portal hypertension, portal vein thrombosis, and hepatorenal syndrome. Cirrhosis are chronic, excessive alcohol use, viral hepatitis, and nonalcoholic steatohepatitis Steatohepatitis Drug-induced Liver Injury (NASH). Decompensation occurs late in the disease with manifestations including jaundice Jaundice Jaundice is the abnormal yellowing of the skin and/or sclera caused by the accumulation of bilirubin. Hyperbilirubinemia is caused by either an increase in bilirubin production or a decrease in the hepatic uptake, conjugation, or excretion of bilirubin. Jaundice , ascites Ascites Ascites is the pathologic accumulation of fluid within the peritoneal cavity that occurs due to an osmotic and/or hydrostatic pressure imbalance secondary to portal hypertension (cirrhosis, heart failure) or non-portal hypertension (hypoalbuminemia, malignancy, infection). Ascites , portal hypertension Portal hypertension Portal hypertension is increased pressure in the portal venous system. This increased pressure can lead to splanchnic vasodilation, collateral blood flow through portosystemic anastomoses, and increased hydrostatic pressure. There are a number of etiologies, including cirrhosis, right-sided congestive heart failure, schistosomiasis, portal vein thrombosis, hepatitis, and Budd-Chiari syndrome. Portal Hypertension , and liver Liver The liver is the largest gland in the human body. The liver is found in the superior right quadrant of the abdomen and weighs approximately 1.5 kilograms. Its main functions are detoxification, metabolism, nutrient storage (e.g., iron and vitamins), synthesis of coagulation factors, formation of bile, filtration, and storage of blood. Liver: Anatomy failure.
- Lower-extremity deep vein thrombosis Deep vein thrombosis Deep vein thrombosis (DVT) usually occurs in the deep veins of the lower extremities. The affected veins include the femoral, popliteal, iliofemoral, and pelvic veins. Proximal DVT is more likely to cause a pulmonary embolism (PE) and is generally considered more serious. Deep Vein Thrombosis ( DVT DVT Deep vein thrombosis (DVT) usually occurs in the deep veins of the lower extremities. The affected veins include the femoral, popliteal, iliofemoral, and pelvic veins. Proximal DVT is more likely to cause a pulmonary embolism (PE) and is generally considered more serious. Deep Vein Thrombosis ): occlusion of a deep vein by a thrombosis Thrombosis Formation and development of a thrombus or blood clot in the blood vessel. Epidemic Typhus , most commonly occurring in the calves Calves Erythema Nodosum . The affected veins Veins Veins are tubular collections of cells, which transport deoxygenated blood and waste from the capillary beds back to the heart. Veins are classified into 3 types: small veins/venules, medium veins, and large veins. Each type contains 3 primary layers: tunica intima, tunica media, and tunica adventitia. Veins: Histology may include the femoral, popliteal, iliofemoral, or pelvic veins Veins Veins are tubular collections of cells, which transport deoxygenated blood and waste from the capillary beds back to the heart. Veins are classified into 3 types: small veins/venules, medium veins, and large veins. Each type contains 3 primary layers: tunica intima, tunica media, and tunica adventitia. Veins: Histology . Hydrostatic pressure Hydrostatic pressure The pressure due to the weight of fluid. Edema increases distal to the DVT DVT Deep vein thrombosis (DVT) usually occurs in the deep veins of the lower extremities. The affected veins include the femoral, popliteal, iliofemoral, and pelvic veins. Proximal DVT is more likely to cause a pulmonary embolism (PE) and is generally considered more serious. Deep Vein Thrombosis , which leads to edema Edema Edema is a condition in which excess serous fluid accumulates in the body cavity or interstitial space of connective tissues. Edema is a symptom observed in several medical conditions. It can be categorized into 2 types, namely, peripheral (in the extremities) and internal (in an organ or body cavity). Edema and pain Pain An unpleasant sensation induced by noxious stimuli which are detected by nerve endings of nociceptive neurons. Pain: Types and Pathways seen on presentation Presentation The position or orientation of the fetus at near term or during obstetric labor, determined by its relation to the spine of the mother and the birth canal. The normal position is a vertical, cephalic presentation with the fetal vertex flexed on the neck. Normal and Abnormal Labor . Ultrasound can visualize the thrombus and anticoagulation Anticoagulation Pulmonary Hypertension Drugs is the primary mode of treatment.
Decreased capillary oncotic pressure Oncotic Pressure Edema
Decreased capillary oncotic pressure Oncotic Pressure Edema (usually due to a loss of albumin Albumin Serum albumin from humans. It is an essential carrier of both endogenous substances, such as fatty acids and bilirubin, and of xenobiotics in the blood. Liver Function Tests ) is the failure to retain fluid within the capillaries, leading to increased capillary leakage. Hypoalbuminemia Hypoalbuminemia A condition in which albumin level in blood (serum albumin) is below the normal range. Hypoalbuminemia may be due to decreased hepatic albumin synthesis, increased albumin catabolism, altered albumin distribution, or albumin loss through the urine (albuminuria). Nephrotic Syndrome in Children may result from:
- Nephrotic syndrome Nephrotic syndrome Nephrotic syndrome is characterized by severe proteinuria, hypoalbuminemia, and peripheral edema. In contrast, the nephritic syndromes present with hematuria, variable loss of renal function, and hypertension, although there is sometimes overlap of > 1 glomerular disease in the same individual. Nephrotic Syndrome : a broad category of glomerular diseases characterized by severe proteinuria Proteinuria The presence of proteins in the urine, an indicator of kidney diseases. Nephrotic Syndrome in Children , hypoalbuminemia Hypoalbuminemia A condition in which albumin level in blood (serum albumin) is below the normal range. Hypoalbuminemia may be due to decreased hepatic albumin synthesis, increased albumin catabolism, altered albumin distribution, or albumin loss through the urine (albuminuria). Nephrotic Syndrome in Children , edema Edema Edema is a condition in which excess serous fluid accumulates in the body cavity or interstitial space of connective tissues. Edema is a symptom observed in several medical conditions. It can be categorized into 2 types, namely, peripheral (in the extremities) and internal (in an organ or body cavity). Edema , and hyperlipidemia. In most cases, a kidney biopsy Biopsy Removal and pathologic examination of specimens from the living body. Ewing Sarcoma is necessary for diagnosis. Management varies with etiology and usually involves glucocorticoids Glucocorticoids Glucocorticoids are a class within the corticosteroid family. Glucocorticoids are chemically and functionally similar to endogenous cortisol. There are a wide array of indications, which primarily benefit from the antiinflammatory and immunosuppressive effects of this class of drugs. Glucocorticoids .
- Cirrhosis Cirrhosis Cirrhosis is a late stage of hepatic parenchymal necrosis and scarring (fibrosis) most commonly due to hepatitis C infection and alcoholic liver disease. Patients may present with jaundice, ascites, and hepatosplenomegaly. Cirrhosis can also cause complications such as hepatic encephalopathy, portal hypertension, portal vein thrombosis, and hepatorenal syndrome. Cirrhosis (above): Severe liver Liver The liver is the largest gland in the human body. The liver is found in the superior right quadrant of the abdomen and weighs approximately 1.5 kilograms. Its main functions are detoxification, metabolism, nutrient storage (e.g., iron and vitamins), synthesis of coagulation factors, formation of bile, filtration, and storage of blood. Liver: Anatomy disease may lead to a decrease in albumin Albumin Serum albumin from humans. It is an essential carrier of both endogenous substances, such as fatty acids and bilirubin, and of xenobiotics in the blood. Liver Function Tests synthesis Synthesis Polymerase Chain Reaction (PCR) .
Increased capillary permeability
Some conditions lead to increases in capillary permeability independent of changes in hydrostatic or oncotic pressure Oncotic Pressure Edema . The conditions are often due to the release Release Release of a virus from the host cell following virus assembly and maturation. Egress can occur by host cell lysis, exocytosis, or budding through the plasma membrane. Virology of inflammatory cytokines Cytokines Non-antibody proteins secreted by inflammatory leukocytes and some non-leukocytic cells, that act as intercellular mediators. They differ from classical hormones in that they are produced by a number of tissue or cell types rather than by specialized glands. They generally act locally in a paracrine or autocrine rather than endocrine manner. Adaptive Immune Response . Some conditions include:
- Sepsis Sepsis Systemic inflammatory response syndrome with a proven or suspected infectious etiology. When sepsis is associated with organ dysfunction distant from the site of infection, it is called severe sepsis. When sepsis is accompanied by hypotension despite adequate fluid infusion, it is called septic shock. Sepsis and Septic Shock : a clinical syndrome resulting from a dysregulated, systemic, host response to infection. Systemic release Release Release of a virus from the host cell following virus assembly and maturation. Egress can occur by host cell lysis, exocytosis, or budding through the plasma membrane. Virology of inflammatory molecules leads to activation of endothelial cells and an increase in capillary permeability. Sepsis Sepsis Systemic inflammatory response syndrome with a proven or suspected infectious etiology. When sepsis is associated with organ dysfunction distant from the site of infection, it is called severe sepsis. When sepsis is accompanied by hypotension despite adequate fluid infusion, it is called septic shock. Sepsis and Septic Shock also results in a significant decrease in the number of functioning capillaries (likely due to compression Compression Blunt Chest Trauma by surrounding tissue edema Edema Edema is a condition in which excess serous fluid accumulates in the body cavity or interstitial space of connective tissues. Edema is a symptom observed in several medical conditions. It can be categorized into 2 types, namely, peripheral (in the extremities) and internal (in an organ or body cavity). Edema ) and plugging of the capillaries by blood cells, which lose their deformability.
- Angioedema Angioedema Angioedema is a localized, self-limited (but potentially life-threatening), nonpitting, asymmetrical edema occurring in the deep layers of the skin and mucosal tissue. The common underlying pathophysiology involves inflammatory mediators triggering significant vasodilation and increased capillary permeability. Angioedema : a localized, self-limited, potentially life-threatening, nonpitting, asymmetrical edema Edema Edema is a condition in which excess serous fluid accumulates in the body cavity or interstitial space of connective tissues. Edema is a symptom observed in several medical conditions. It can be categorized into 2 types, namely, peripheral (in the extremities) and internal (in an organ or body cavity). Edema occurring in the deep layers of the skin Skin The skin, also referred to as the integumentary system, is the largest organ of the body. The skin is primarily composed of the epidermis (outer layer) and dermis (deep layer). The epidermis is primarily composed of keratinocytes that undergo rapid turnover, while the dermis contains dense layers of connective tissue. Skin: Structure and Functions and mucosal tissue. The common underlying pathophysiology involves inflammatory mediators, which trigger Trigger The type of signal that initiates the inspiratory phase by the ventilator Invasive Mechanical Ventilation significant vasodilation Vasodilation The physiological widening of blood vessels by relaxing the underlying vascular smooth muscle. Pulmonary Hypertension Drugs and increased capillary permeability. Angioedema Angioedema Angioedema is a localized, self-limited (but potentially life-threatening), nonpitting, asymmetrical edema occurring in the deep layers of the skin and mucosal tissue. The common underlying pathophysiology involves inflammatory mediators triggering significant vasodilation and increased capillary permeability. Angioedema presentation Presentation The position or orientation of the fetus at near term or during obstetric labor, determined by its relation to the spine of the mother and the birth canal. The normal position is a vertical, cephalic presentation with the fetal vertex flexed on the neck. Normal and Abnormal Labor includes swelling Swelling Inflammation around the eyes, lips Lips The lips are the soft and movable most external parts of the oral cavity. The blood supply of the lips originates from the external carotid artery, and the innervation is through cranial nerves. Lips and Tongue: Anatomy , tongue Tongue The tongue, on the other hand, is a complex muscular structure that permits tasting and facilitates the process of mastication and communication. The blood supply of the tongue originates from the external carotid artery, and the innervation is through cranial nerves. Lips and Tongue: Anatomy , mouth, bowel wall, extremities, or genitalia. The airway Airway ABCDE Assessment may be compromised.
- Idiopathic Idiopathic Dermatomyositis systemic capillary leak syndrome Capillary leak syndrome A condition characterized by recurring episodes of fluid leaking from capillaries into extravascular compartments causing hematocrit to rise precipitously. If not treated, generalized vascular leak can lead to generalized edema; shock; cardiovascular collapse; and multiple organ failure. Hematopoietic Growth Factors : a rare disorder characterized by episodes of severe hypotension Hypotension Hypotension is defined as low blood pressure, specifically < 90/60 mm Hg, and is most commonly a physiologic response. Hypotension may be mild, serious, or life threatening, depending on the cause. Hypotension , hypoalbuminemia Hypoalbuminemia A condition in which albumin level in blood (serum albumin) is below the normal range. Hypoalbuminemia may be due to decreased hepatic albumin synthesis, increased albumin catabolism, altered albumin distribution, or albumin loss through the urine (albuminuria). Nephrotic Syndrome in Children , and hemoconcentration Hemoconcentration Neonatal Polycythemia . The etiology is unknown. Clinical presentation Presentation The position or orientation of the fetus at near term or during obstetric labor, determined by its relation to the spine of the mother and the birth canal. The normal position is a vertical, cephalic presentation with the fetal vertex flexed on the neck. Normal and Abnormal Labor results from systemic, capillary leakage of fluid with protein and larger molecule retention within the vessels.
Other clinical conditions associated with abnormal capillaries
- Diabetes mellitus Diabetes mellitus Diabetes mellitus (DM) is a metabolic disease characterized by hyperglycemia and dysfunction of the regulation of glucose metabolism by insulin. Type 1 DM is diagnosed mostly in children and young adults as the result of autoimmune destruction of β cells in the pancreas and the resulting lack of insulin. Type 2 DM has a significant association with obesity and is characterized by insulin resistance. Diabetes Mellitus : Chronic hyperglycemia Hyperglycemia Abnormally high blood glucose level. Diabetes Mellitus can cause diabetic microangiopathy, a thickening of the capillary basal lamina reducing the metabolic exchange between blood and tissues. The microangiopathy may ultimately lead to tissue ischemia Ischemia A hypoperfusion of the blood through an organ or tissue caused by a pathologic constriction or obstruction of its blood vessels, or an absence of blood circulation. Ischemic Cell Damage (especially in the kidneys Kidneys The kidneys are a pair of bean-shaped organs located retroperitoneally against the posterior wall of the abdomen on either side of the spine. As part of the urinary tract, the kidneys are responsible for blood filtration and excretion of water-soluble waste in the urine. Kidneys: Anatomy , eyes, and limbs) and result in renal failure Renal failure Conditions in which the kidneys perform below the normal level in the ability to remove wastes, concentrate urine, and maintain electrolyte balance; blood pressure; and calcium metabolism. Renal insufficiency can be classified by the degree of kidney damage (as measured by the level of proteinuria) and reduction in glomerular filtration rate. Crush Syndrome , blindness Blindness The inability to see or the loss or absence of perception of visual stimuli. This condition may be the result of eye diseases; optic nerve diseases; optic chiasm diseases; or brain diseases affecting the visual pathways or occipital lobe. Retinopathy of Prematurity , and/or limb amputations, respectively.
- Telangiectasia Telangiectasia Permanent dilation of preexisting blood vessels creating small focal red lesions, most commonly in the skin or mucous membranes. It is characterized by the prominence of skin blood vessels, such as vascular spiders. Chronic Venous Insufficiency : Small, dilated blood vessels (usually arterioles Arterioles The smallest divisions of the arteries located between the muscular arteries and the capillaries. Arteries: Histology , venules Venules The minute vessels that collect blood from the capillary plexuses and join together to form veins. Veins: Histology , or capillaries) appear as thin, red lines on the skin Skin The skin, also referred to as the integumentary system, is the largest organ of the body. The skin is primarily composed of the epidermis (outer layer) and dermis (deep layer). The epidermis is primarily composed of keratinocytes that undergo rapid turnover, while the dermis contains dense layers of connective tissue. Skin: Structure and Functions or mucous membranes.
References
- Taylor, A.M., and Bordoni, B. (2021). Histology, blood vascular system. In StatPearls. Retrieved April 26, 2021, from https://www.ncbi.nlm.nih.gov/books/NBK553217/
- Saladin, K.S., Miller, L. (2004). Anatomy and physiology. (3rd Ed., Pp. 750‒752).
- Moore, K.L., and Dalley, A.F. (2006). Clinically oriented anatomy. (5th Ed., Pp 44).
Source: https://www.lecturio.com/concepts/capillaries/
Post a Comment for "Continuous Fenestrated and Sinusoidal Describe a Type of Capillary"